We all recognize the term “20/20 vision.” But what does 20/20 vision mean exactly? That’s what we will get into in this blog.
Plus, we will dive into what other kinds of visions there are and what they mean. Also, we’ll help you understand visual acuity and how doctors use the Snellen eye chart to diagnose eyesight conditions.
Eyesurgeryclinics.org provides several monthly blogs on eye-related topics. If you have an issue with your vision, you can read and learn more about it on our website. We aim to help those with sight problems identify and understand their condition. We’re also an educational guide for aspiring optometrists and eye professionals.
20/20 Vision Definition
Firstly, what does 20/20 vision mean? Let’s start with the term visual acuity.

Visual acuity is the measure of how sharp your eyesight is. The standard eyesight test that determines your eyes’ sharpness takes place at a distance of twenty feet. The term 20/20 vision is what optometrists use to define normal vision. If you can see items and objects clearly from twenty feet away, doctors will deem you have 20/20 vision.
Visual acuity tests can be thorough, and they don’t always only test your forward vision. They may extend to your coordination, peripheral vision, focus, and depth perception. Doctors will have you look at various size letters from different angles to gauge your vision level.
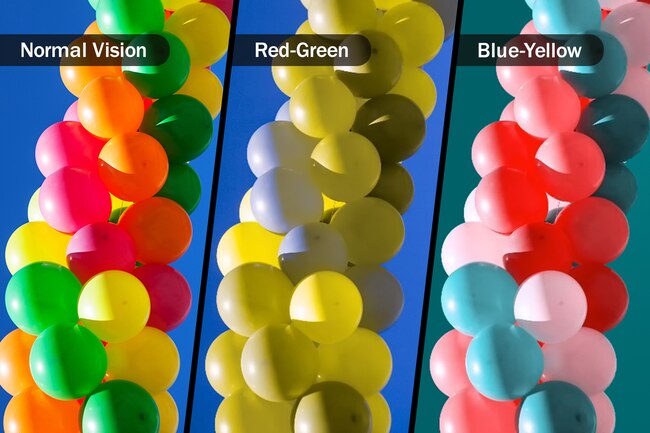
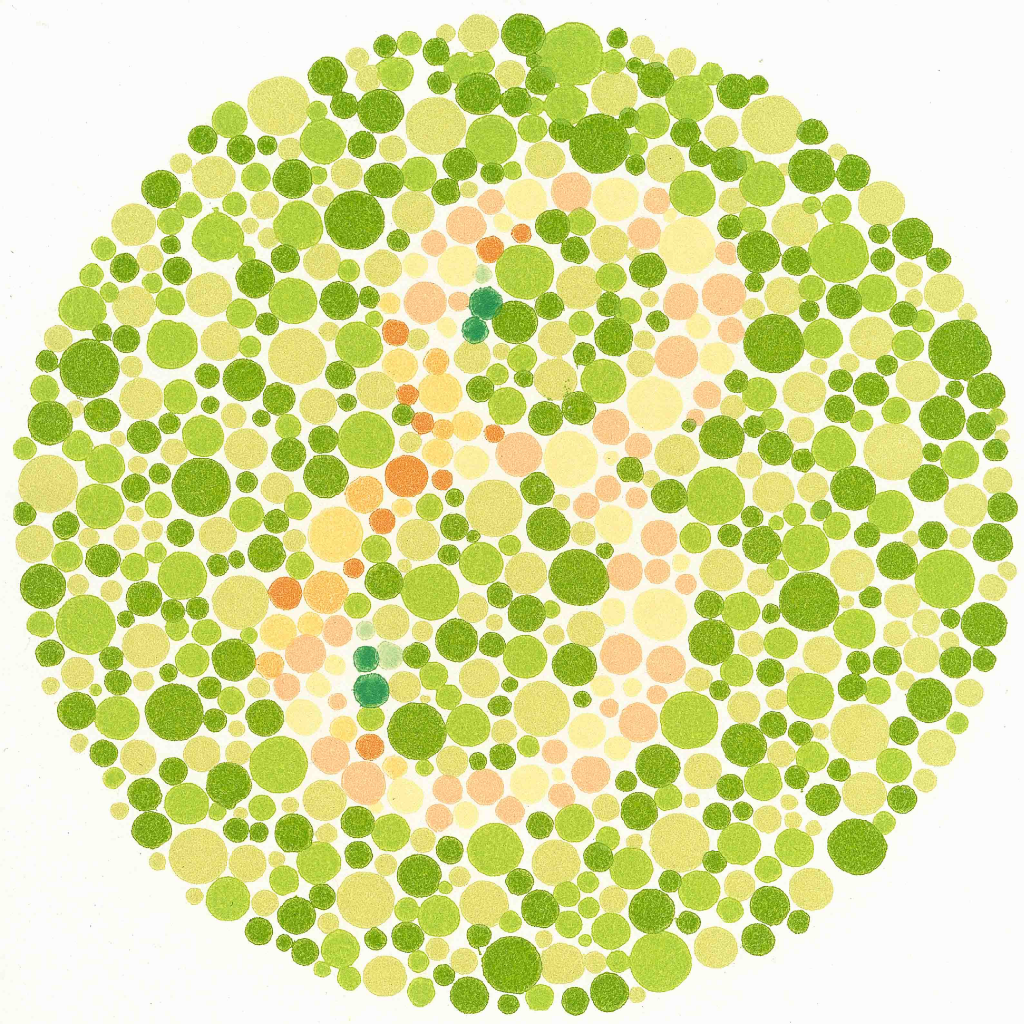
Even with in-depth testing, it can be hard to predict some eyesight issues you may have. For example, you may have trouble differentiating between colors and reading text with monochromatic backgrounds despite having 20/20 vision.
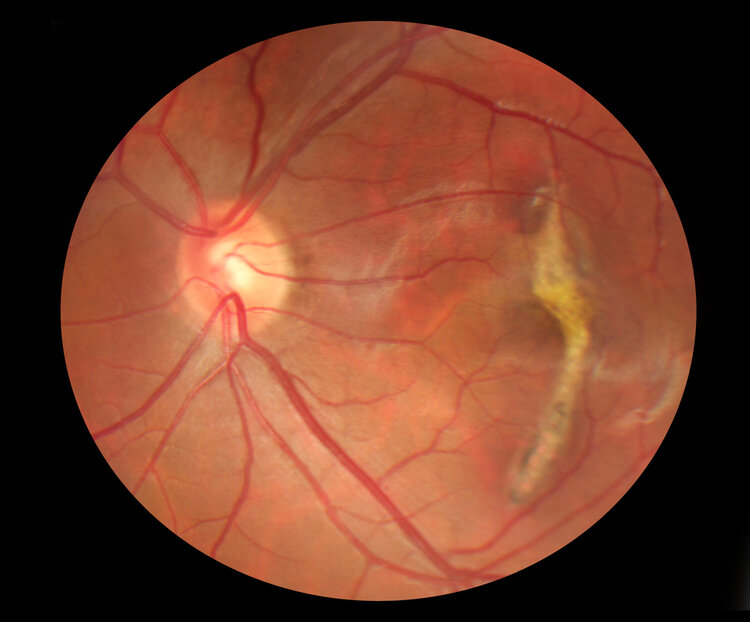
There are a few things that make for healthy visual acuity. Your cornea and lens’s job is to reflect light onto your retina. The efficiency of the lens and cornea dictates how sharp your vision is. Nerve sensitivity is also a factor in your visual acuity. Your nerves help protect your eye and allow you to process most visuals instantly.
People with clear eyesight do not require prescription glasses. However, as you get older, your sight may become worse. Just because you have 20/20 vision today doesn’t mean it will remain that way for the rest of your life.
You need to prove you have 20/20 vision to work some jobs. For example, 20/20 vision is the minimum eye strength that pilots need to fly a plane.
The Snellen Eye Chart
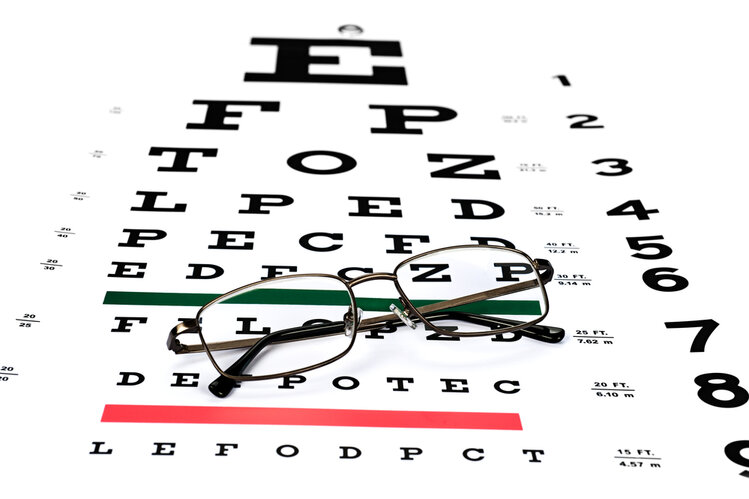
Though you may not recognize the name, most everyone knows what the Snellen eye chart is. Typically, your doctor or optometrist will place the Snellen chart in front of you and have you cover one eye. The chart has letters of all sizes, with the top row being the largest and the bottom row the smallest. You read the letters aloud, row by row.
This test is how doctors evaluate the sharpness of your vision. If you reach the eighth row of letters, your optometrist will determine that you have 20/20 vision. Doctors use this chart to diagnose a few different eye conditions. If you fail the test, you may require prescription glasses.
20/20 Variations
There are many different types of vision aside from 20/20. Firstly, there’s 20/15 eyesight. This level is better than its 20/20 counterpart. A person with 20/15 vision can see an item at twenty feet, what a person with 20/20 vision can only see standing fifteen feet away. Thus, people with 20/15 vision have better eyesight than those with 20/20.
Alternatively, there is 20/40 vision. Most everyone has at least this level of sight. It is the minimum eyesight you need to obtain a driver’s license in all fifty states. If you have lower than 20/40 vision, you will have difficulty reading books, paperwork, or any printed material.
Further down the line, we have 20/80 vision. An item on this level of eyesight is newspaper headlines. While not legally blind at 20/80, optometrists consider people with 20/80 moderately visually impaired, and you would require prescription glasses.
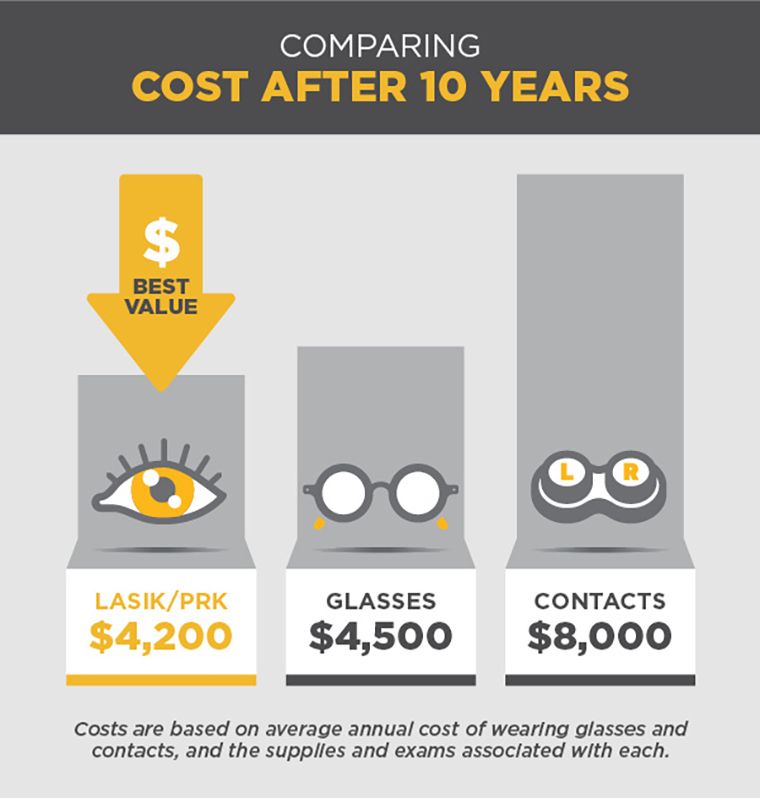
In some cases, you can correct 20/80 vision with eye surgery. Consult your optometrist about possible corrective procedures. Eyeglass technology has come a long way and is better than ever, and corrective eye surgery is becoming more common for those looking for a more permanent solution.
Finally, there is 20/200 vision. Optometrists will require you to wear eyewear at this level of sight. Plus, they will consider you legally blind. You need to stand twenty feet away from what people with 20/20 vision can see from 200 feet. However, people with 20/200 vision can still live a high-quality life.
Is 20/20 Vision Perfect?
Contrary to popular belief, 20/20 vision does not mean that you have perfect sight. Optometrists consider people with 20/20 vision to have normal eyesight.
It is possible to have more than 20/20 vision. People with this level of visual prowess may have some flaws in their peripheral vision or coordination. Your optometrist will let you know if your eyes need further evaluation after your Snellen test.
Many people who want to improve their eyesight turn to LASIK, a laser correction procedure. Ask your ophthalmologist about laser treatment to see if it is right for you. If it is, your ophthalmologist can refer you to a LASIK surgeon.
There are also eye specialists for athletes who feel their vision when playing sports is weak. Your optometrist can refer you to a sports specialist who can better diagnose your condition.
Read More
Most people have 20/20 vision. However, it is not a problem if you do not. As we get older, our eyesight diminishes, which is a part of life. The crucial thing is not to let it impact your day-to-day routine. With the proper treatment, you can find a way to cope with your eye disorder.
If you enjoy this article, feel free to browse more of our informational guides about other eye-related topics. We strive to help you learn all there is to know about eye conditions and terminology. Each year, we help thousands of people learn more about their eyesight issues and lead them on the path toward treatment.